Diagnostic Reasoning: Chest Pain Framework
The System 1 Trap
It’s 3am on AMU and you’re called to see a 58-year-old man with chest pain that is central, crushing, and radiating to his left arm. He’s sweating, looks grey, and tells you it feels like “an elephant sitting on my chest.”
Your brain immediately locks onto one diagnosis: MI.
You’re probably right. The troponins will likely confirm it. But what if you’re wrong? What if it’s the one presentation that looks exactly like an MI but isn’t? What if it’s aortic dissection, and you’ve just given aspirin?
This is where System 1 thinking (fast, pattern-matching, instinctive) can lead you astray. It’s brilliant for speed, but dangerous when it makes you stop thinking. System 1 thinking is your clinical autopilot. You hear “crushing central chest pain” and your brain instantly pattern-matches: MI. ECG. Troponin. Aspirin. Done.
This works most of the time. That’s why it evolved. But the issue with System 1 thinking is that it stops looking once it finds a match. It doesn’t ask “what else could this be?” It certainly doesn’t ask “what will kill this patient if I’m wrong?” It’s not that System 1 is wrong, consultants use this type of thinking all the time, which is how they can see so many patients quickly. But it’s incomplete. You need a way to quickly and systematically rule out the other killers, even when MI seems obvious.
That’s where the chest pain framework comes in.
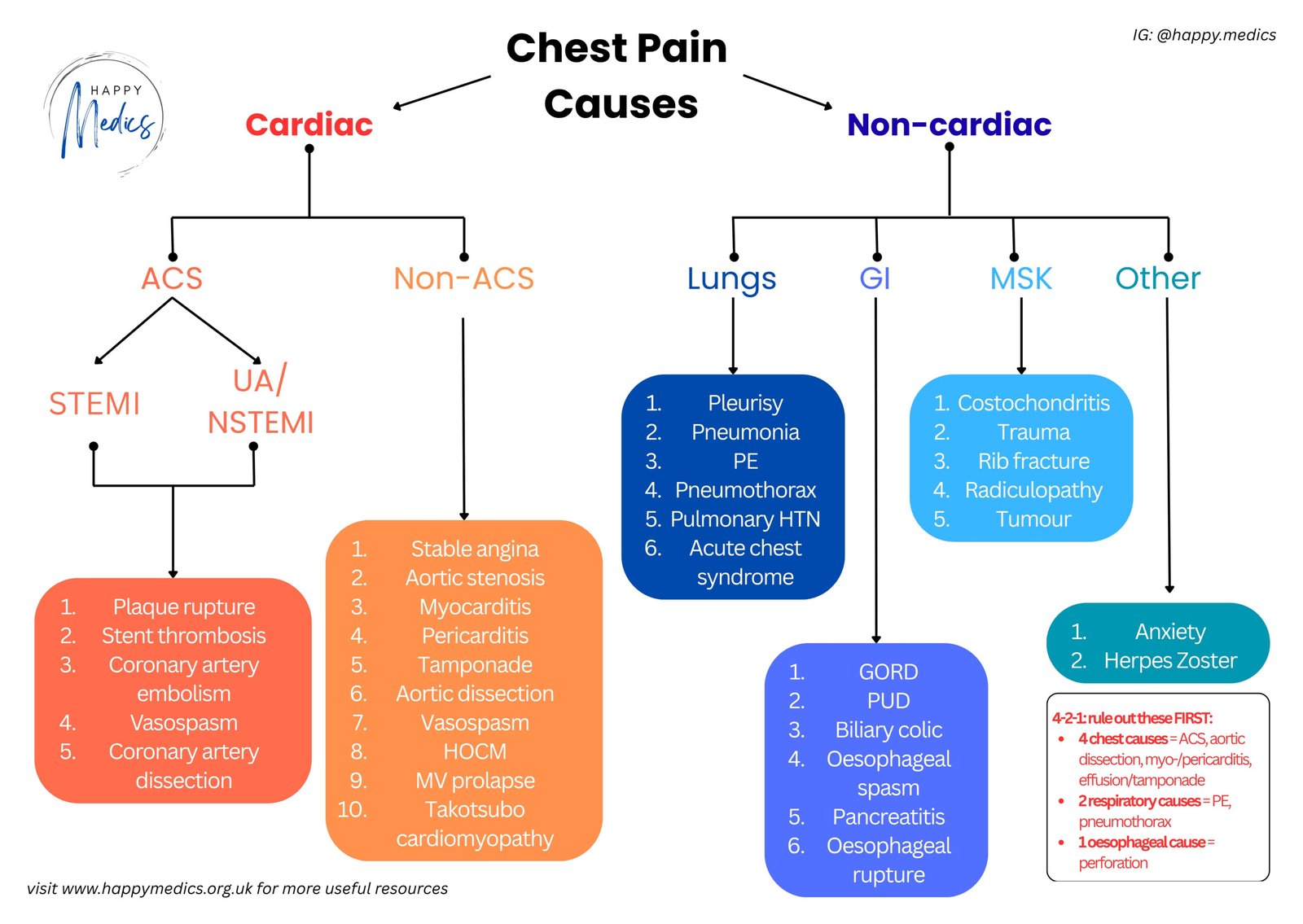
The 4-2-1 Framework for Chest Pain
I use this for every chest pain presentation. It forces me to pause System 1 just long enough to check for the most urgent to rule out scenarios.
4 Cardiac Causes:
- MI (your System 1 favourite)
- Aortic dissection (the MI mimic that aspirin will make worse)
- Pericarditis/Myocarditis (can look identical on ECG sometimes)
- Cardiac tamponade (rare, but rapidly fatal if missed)
2 Pulmonary Causes:
- Pulmonary embolism (especially if there’s breathlessness)
- Tension pneumothorax (listen to the chest, always)
1 Gastrointestinal Cause:
- Oesophageal rupture/spasm/impaction (the great pretender)
These aren’t every cause of chest pain, but they are the causes that matter urgently, i.e. the ones you cannot afford to miss.
Everything else can wait.
When 4-2-1 isn’t enough: When the presentation is atypical or 4-2-1 doesn’t clarify things, you’ll need the comprehensive chest pain framework. It breaks down cardiac causes into ACS vs non-ACS, then covers respiratory, GI, MSK, and other causes systematically. Think of 4-2-1 as your rapid screen for immediate threats, whereas the comprehensive framework is your backup for complex cases.
The Chest Pain Framework in Action
Back to our 58-year-old. You’re thinking MI. Let’s walk through 4-2-1 systematically while the ECG is being done.
4 Cardiac:
- MI? Classic presentation, high probability. ECG will confirm.
- Dissection? Ask about sudden onset, tearing quality, radiation to the back. Check BP in both arms—a difference >20mmHg is a red flag (this test is quick and free). Any prior history of hypertension or connective tissue disease?
- Pericarditis? Does the pain change with position or breathing? Pericarditis is usually sharp and positional, but it can surprise you.
- Tamponade? Check JVP, listen for muffled heart sounds, look for pulsus paradoxus. It’s rare, but if you don’t think of it, you won’t find it.
2 Pulmonary:
- PE? Any breathlessness disproportionate to the pain? Recent surgery, long flight, leg swelling? Wells score if suspicious.
- Pneumothorax? Reduced air entry on one side? Sudden onset? Examine the chest properly, don’t just listen to the heart, and consider a chest X-ray.
1 Gastrointestinal:
- Oesophageal? Recent vomiting? Difficulty swallowing? Subcutaneous emphysema in the neck? (Oesophageal rupture is surgical and rapidly fatal if missed.)
After all that, you’re still thinking MI. The ECG comes back and shows ST elevation – you were right. But now you’ve also systematically excluded the other killers in under five minutes.
And if the ECG had been normal? You’d still have your differential ready to work through.
Key Actions: What You Must Do
When you’re assessing chest pain, these are non-negotiable:
- Get an ECG immediately: Don’t delay for a full history—you can take history while the ECG is being done. Time is myocardium.
- Examine properly: Listen to the chest, feel both radial pulses simultaneously, check BP in both arms if dissection is remotely possible.
- Think in parallel, not sequentially: While the ECG is happening, secure IV access, give aspirin (if no dissection concerns), arrange monitoring, check observations. Don’t wait for one thing to finish before starting the next.
- Ask the killer question: “What will kill this patient in the next hour if I’m wrong?” This single question activates System 2 thinking every time.
Reference: NICE guidelines for management of ACS
Three Things to Remember
✓ Use 4-2-1 every single time – even when MI seems obvious (especially when MI seems obvious)
✓ System 1 gets you to the likely diagnosis quickly; System 2 makes sure you haven’t missed the fatal one
✓ The ECG can happen while you take history – don’t waste time on perfect chronological histories when a patient might be having an MI
About the Author:
Dr Ahmed Kazie is a resident doctor in Acute Medicine and founder of Happy Medics. He teaches systematic diagnostic reasoning through clinical frameworks, helping other resident doctors build confidence in managing acute presentations.
Instagram | Subscribe to Newsletter | Join the AMC Waitlist
